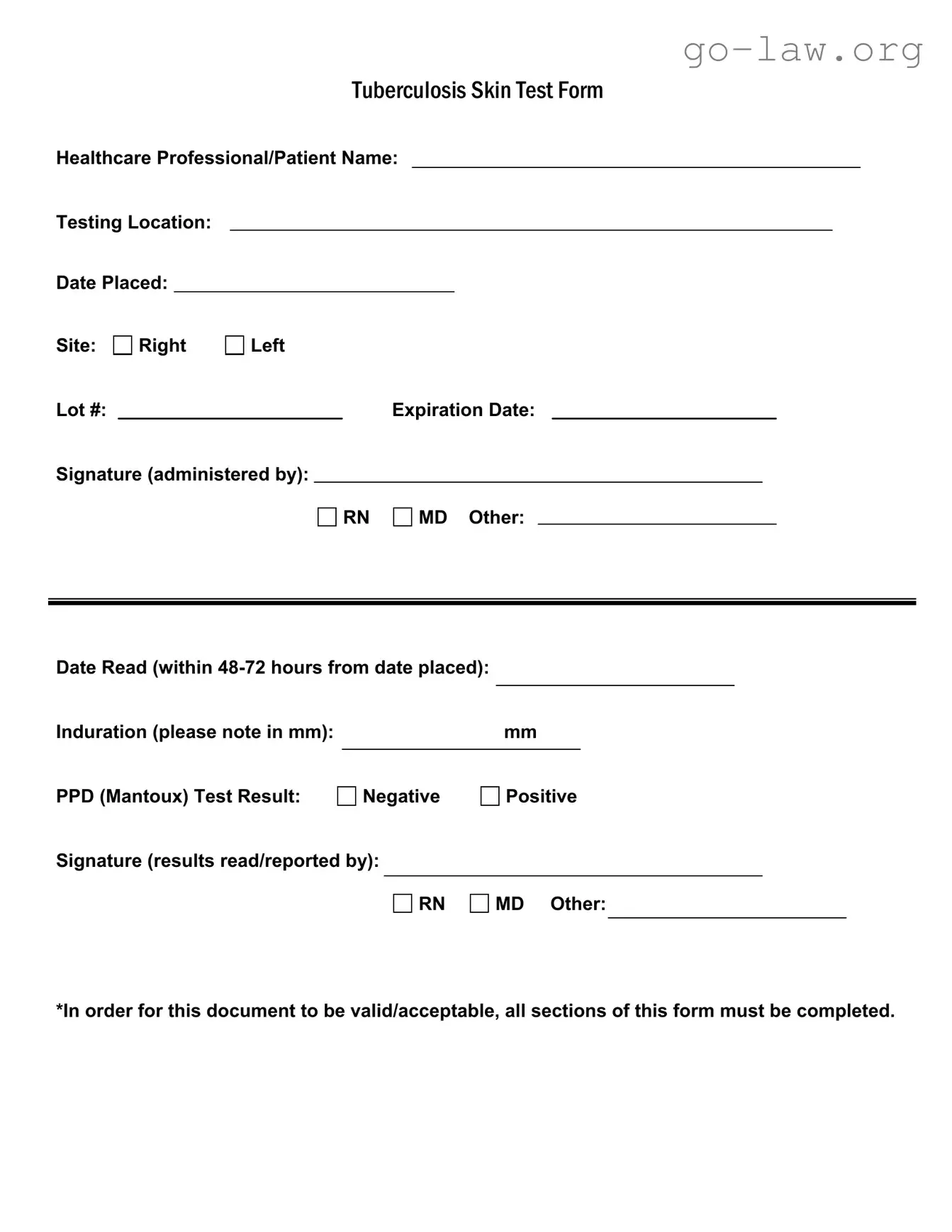
The Tuberculosis (TB) Skin Test Form is a crucial document used in healthcare settings to record essential information regarding TB testing. It includes the names of both the healthcare professional and the patient, ensuring clear identification of those involved in the testing process. The form specifies the testing location and the date the test was placed, which are vital for tracking and follow-up purposes. Additionally, it requires the site of the test to be indicated, allowing for precise documentation. A lot number and expiration date are also necessary, as they confirm the validity of the testing materials used. The signature of the administering professional—whether a registered nurse (RN), medical doctor (MD), or other qualified personnel—is required to authenticate the procedure. After the test is read, typically within 48 to 72 hours, the induration measurement in millimeters must be recorded, followed by the result of the PPD (Mantoux) test, which can be either negative or positive. The form concludes with a signature from the individual who read and reported the results, further ensuring accountability. For the document to be valid and acceptable, it is imperative that all sections are completed thoroughly.